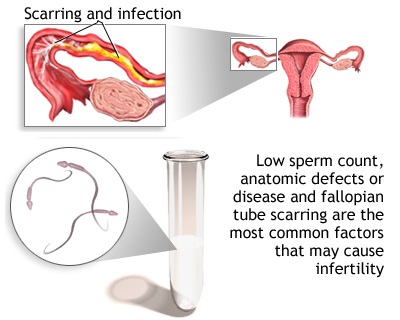
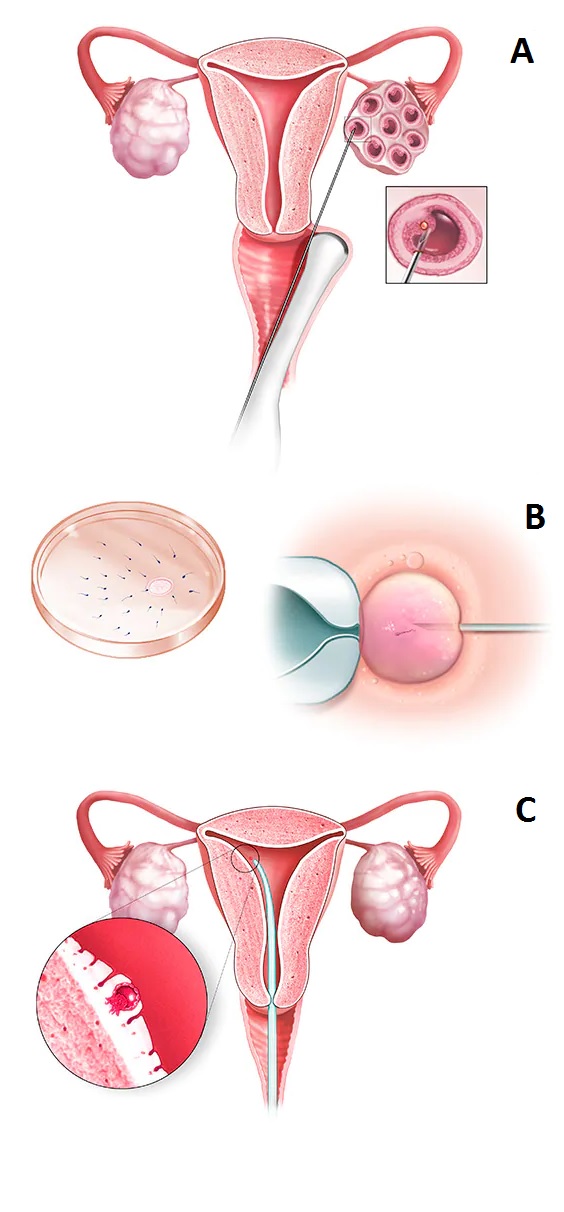
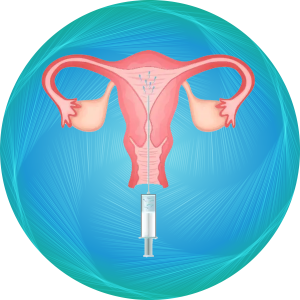
Blocked fallopian tubes or an abnormal uterine cavity may cause infertility.
Hysterosalpingography, or HSG, is an X-ray test to outline the internal shape of the uterus and show whether the fallopian tubes are blocked.
In HSG, a thin tube is threaded through the vagina and cervix. A substance known as contrast material is injected into the uterus.
A series of X-rays, or fluoroscopy, follows the dye, which appears white on X-ray, as it moves into the uterus and then into the tubes. If there is an abnormality in the shape of the uterus, it will be outlined.
If the tube is open, the dye gradually fills it. The dye spills into the pelvic cavity, where the body resorbs it.
العربية
العربية
العربية