Read More
Read More
HomeCategory
Blog Archives | IRANMEDTOUR
 Read More
Read More
 Read More
Read More
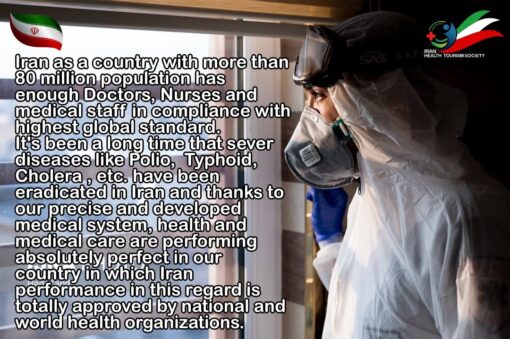
The Iranian medical system, in full force, against the Coronavirus
The Iranian medical system, in full force, against the Coronavirus Iran as a country with…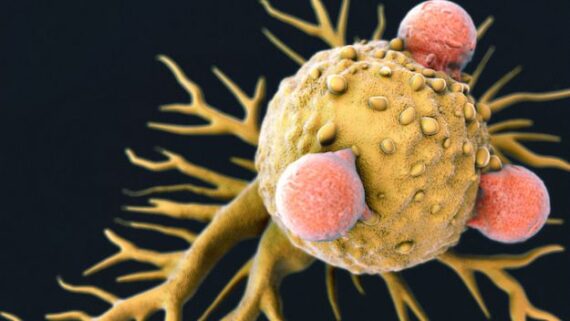 Read More
Read More
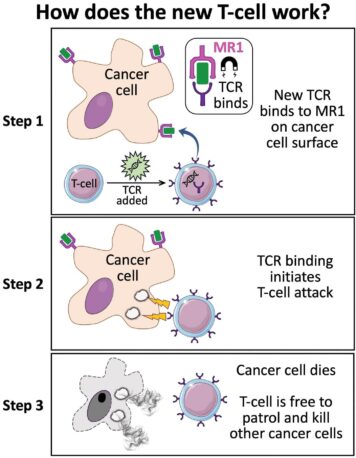
Killer T-Cell Discovery Could Mean ‘Universal’ Cancer Treatment
Killer T-Cell Discovery Could Mean ‘Universal’ Cancer Treatment A new type of killer T-cell could… Read More
Read More
What is Ozone Therapy?
What is Ozone Therapy? Ozone is a colorless gas made up of three oxygen atoms.… Read More
Read More
Who Is Traveling to Iran for Medical Care?
Who Is Traveling to Iran for Medical Care? Iran, and more specifically Tehran, has now… Read More
Read More
Why Are Medical Tourists Choosing Iran?
Why Are Medical Tourists Choosing Iran? Iran is quickly becoming the next international medical tourism… Read More
Read More